
Feeding Patients in the Dark
0 Comments
Submit a Comment
You must be logged in to post a comment.
Related Articles: CMS Rules for Healthcare Providers
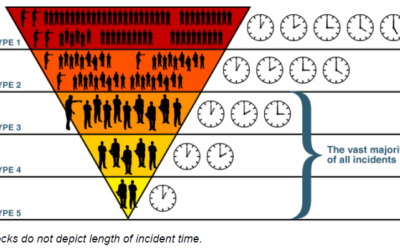
Goldilocks Would Love Incident Command
Incident Command structure should always be “just right” for the incident. It’s a modular system, not all-or-nothing!
Annual Review of Emergency Preparedness Plan
by Rick Christ Current CMS Emergency Preparedness Conditions of Participation require an annual review of your emergency preparedness plan. Under the proposed rule, the plan “must be evaluated and updated at least every 2 years.” Not in the rule, but in...
Why We Support More Detailed Exercise Standards
by Rick Christ Currently, almost every provider type is required to participate in two exercises per year. One “should be” a “community full-scale exercise” while the other can be a tabletop. The original version of the current exercise standards was...
Do the Proposed Changes to Training Make Sense?
by Rick Christ Currently, the typical CMS regulation says this about the training requirement: The training and testing program must be reviewed and updated at least annually. (1) Training program. The hospital must do all of the following:(i) Initial...
Documentation of Cooperation and Collaboration
What You Need to Know About the Proposed Rule Changes to CMS
by Rick Christ Barely ten months into the enforcement period of the Emergency Preparedness Conditions of Participation, the Centers for Medicare and Medicaid Services (CMS) is proposing some rule changes that would “reform Medicare regulations that are...
CMS Compliance Products & Services
[/et_pb_shop]
[/et_pb_shop]
[/et_pb_shop]
Our Newsletter
Remember, we will NEVER share your email address or SPAM you.
You may unsubscribe at any time.
Website design & development by Carbon Six Digital Marketing Agency





We'd Love to Hear Your Comments